The menstrual cycle is the most intricate biological process in the female body system. In addition, an understanding of how hormones are able to regulate such a complicated system allows women to better control their reproductive health. Secondly, the menstrual cycle is a process involving multiple hormone interactions influencing not just reproductive function but also mood, energy levels, and overall well-being.
Hormones are chemical messengers during menstrual cycle phases. Additionally, the functional chemicals transmit between the ovaries, brain, and uterus to maintain normal cycles. Consequently, any disruption in hormone balance could lead to symptoms and abnormal cycles. Accordingly, studying the functions of hormones in the menstrual cycle enlightens women to recognize normal and abnormal cycles.
Stages of the Menstrual Cycle
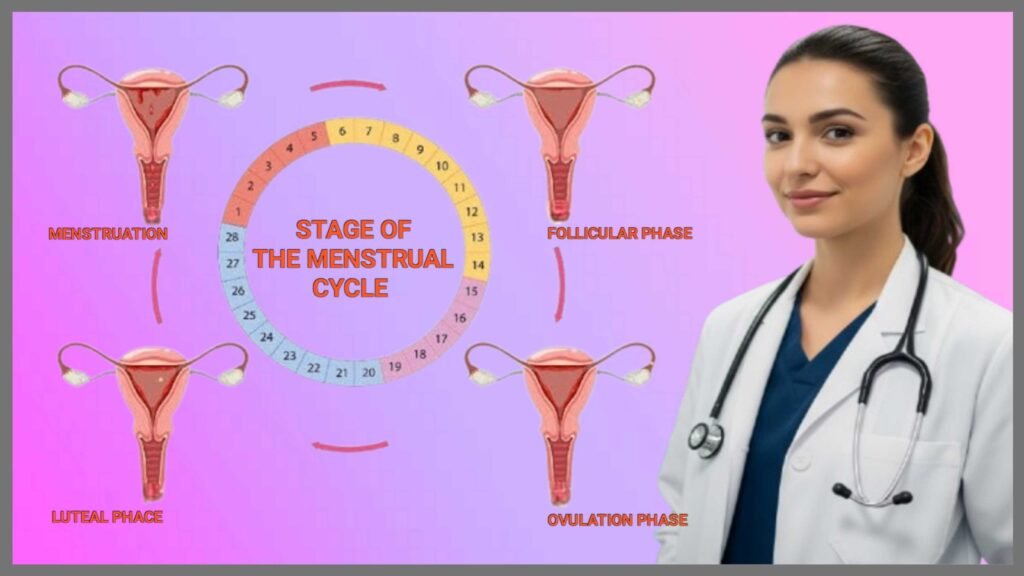
Follicular Phase: Getting Ready to Potentially Be Pregnant
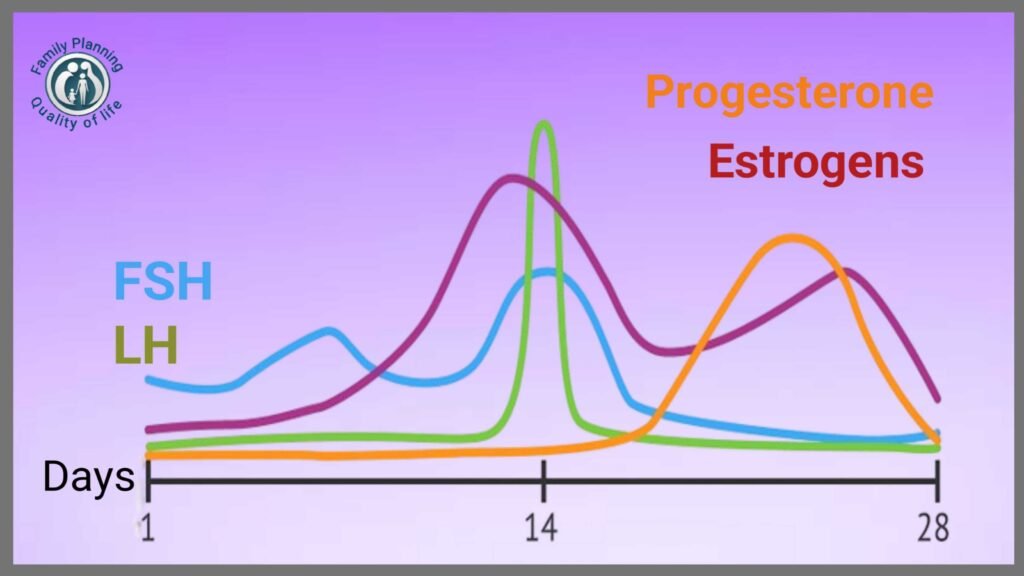
The menstrual cycle is comprised of four different phases that function in balance. Menstrual phase begins with the initial bleeding, cycle day one. After menstruation comes the follicular phase, where preparations for potential conception begin. Next comes ovulation on approximately day fourteen in a normal twenty-eight-day cycle. Last comes the luteal phase to complete the cycle before menstruation once again.
During the follicular phase, follicle-stimulating hormone (FSH) increases significantly. As a result, the hormone causes several follicles in the ovaries to mature. At the same time, estrogen slowly rises as the lead follicle enlarges. The uterine lining also starts rebuilding during the proliferative phase.
Ovulation: The Release Key
Ovulation is the most critical stage in the stages of the menstrual cycle. At this critical moment, luteinizing hormone (LH) experiences a rapid surge that causes the release of the matured egg. Additionally, the LH surge occurs approximately thirty-six hours before ovulation takes place. Surprisingly, estrogen’s level is at its peak just before ovulation, then drops sharply.
To most women, the luteal phase is always fourteen days long. During this period, progesterone and small quantities of estrogen are secreted by the corpus luteum. When there is no pregnancy, hormone levels plummet. This withdrawal of hormones then triggers menstruation to resume and the cycle to repeat.
Also Read : A Comprehensive Guide to Contraception Methods (2025)
Hormonal Imbalance Symptoms
Atypical Bleeding Patterns
Hormonal imbalance within the menstrual cycle can present itself in some uncomfortable symptoms. Firstly, irregular menses usually point to underlying hormonal disturbances in the cycle timing. Secondly, abnormally heavy or abnormally light bleeding patterns can also be a sign of hormonal disturbances. Thirdly, not menstruating for consecutive months usually points to extreme hormonal imbalances and needs medical intervention.
Mood symptoms are commonly explained by hormonal imbalance during the menstrual cycle. For instance, excessive mood swings, depression, or anxiety may be a manifestation of hormonal disturbance. Similarly, excessive irritability or emotional instability typically represents unstable fluctuating hormone levels. In addition, persistent weakness and fatigue may be brought about by hormonal imbalance.
Physical Warning Signs
Physical symptoms of hormonal imbalance include weight change and skin problems without an apparent cause. Specifically, weight gain or difficulty losing weight can be indicators of hormonal imbalance. Furthermore, long-standing acne, excess hair growth, or hair loss are common indicators of hormonal disruption. Furthermore, breast tenderness, bloating, and gastrointestinal issues usually accompany hormonal imbalance.
Hormonal imbalance is also indicated by trouble with regulating temperature and sleep disturbances. In particular, insomnia or sleep quality can be brought about by changes in hormones. Similarly, hot flashes or night sweats which are not experienced during menopause signify hormonal imbalance. Monitoring these symptoms, therefore, picks up patterns in line with the menstrual cycle.
Also Read : Fertility Tracking: Your Path to Success Pregnancy (2025)
Progesterone and Estrogen in Menstrual Cycle
Estrogen: The Architect of Cycle’s First Half
Estrogen and progesterone are the most important female hormones responsible for controlling the menstrual cycle. First of all, estrogen prevails at the beginning of the cycle during the growth of the follicles. That is, estrogen increases reliably from day one to just before ovulation begins. Furthermore, estrogen also causes thickening of the uterine lining in preparation for pregnancy.
Estrogen influences other body systems beyond the reproductive system when we are in the menstrual cycle. For instance, estrogen influences bone density, cardiovascular health, and brain activity. Additionally, the hormone influences skin elasticity, mood, and levels of energy. Moreover, estrogen sensitizes the body to insulin and maintains cholesterol under control.
Progesterone: The Luteal Phase Guardian
Progesterone is front and center during the luteal phase after ovulation. Interestingly, progesterone increases dramatically after successful corpus luteum formation and ovulation. This steroid hormone plays a critical role in maintaining the optimal conditions within the uterine lining for possible adhesion of an embryo. Progesterone does have sedative effects, though, that sometimes cause additional sleepiness.
The interactive equilibrium between estrogen and progesterone manages the entire menstrual cycle experience. Cycles are normal and manageable when the two hormones are perfectly balanced. Conversely, a lack of balance between estrogen and progesterone can result in many problems. Perfect reproductive health relies on proper hormonal balance.
Also Read : Preconception Health: Essential Guide to Pregnancy Prep (2025)
How Your Hormones Affect Your Period
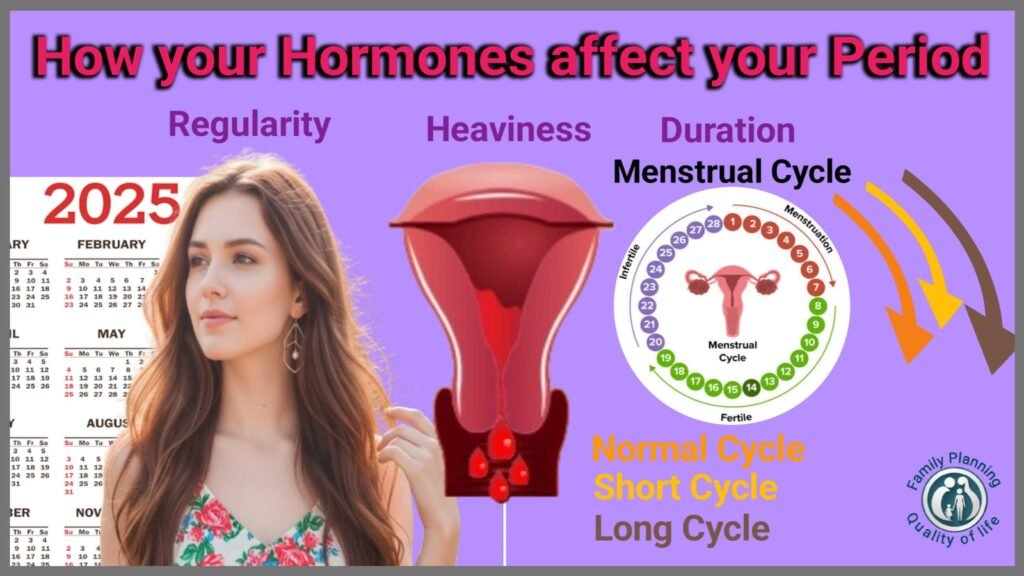
Hormonal Reasons for Menstruation
Hormones control each phase of your menstrual cycle, from timing to flow. The initial drop in estrogen and progesterone causes menstruation to begin first. That hormonal shift is then followed by prostaglandins, causing contractions of the uterine muscles that enable endometrial tissue to be removed. These hormone-like substances also cause cramping and pain with menstruation.
Hormonal changes during the menstrual cycle have a profound effect on menstruation parameters during every month. For example, the levels of estrogen regulate the thickness of the uterine lining. Hence, high estrogen will lead to heavier periods with thicker endometrial tissue, and low estrogen may lead to lighter, shorter periods.
Stabilization Role of Progesterone
Progesterone is one of the stabilizing hormones of the endometrium lining during menstruation. Specifically, adequate progesterone prevents excessive loss and prolonged duration of menstruation. Progesterone deficiency, conversely, causes unpredictable bleeding patterns. Moreover, progesterone withdrawal triggers the inflammatory process to begin menstrual flow.
Hormonal contraceptives illustrate the influence of external hormones on menstrual cycles significantly. Birth control tablets with man-made estrogen and progesterone will change natural cycles. Similarly, hormone-releasing intrauterine devices can significantly reduce menstrual loss or even eliminate periods altogether. Thus, hormone effects explainmanent impacts of contraceptives.
Also Read : Reproductive Health Education: A Guide for Families (2025)
Menstrual Cycle Hormones Explained
GnRH: The Conductor Master
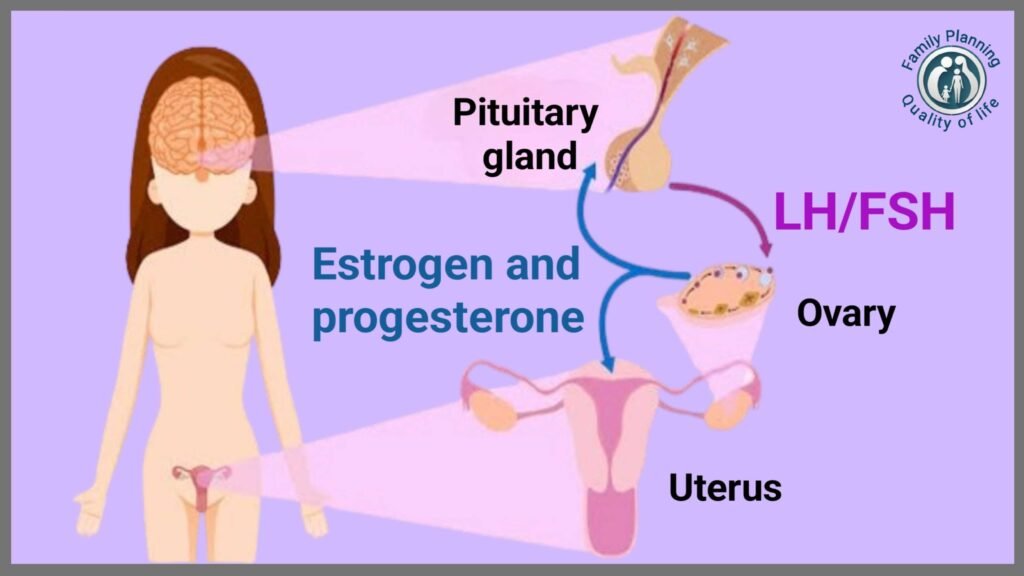
The menstrual cycle is a delicate hormonal symphony that requires accurate timing and coordination. The hypothalamus stimulates the release of gonadotropin-releasing hormone (GnRH), which initiates the entire cycle. GnRH stimulates the release of FSH and LH from the pituitary gland. The gonadotropins then travel to the ovaries to stimulate hormone secretion.
FSH: Follicle Stimulation Expert
FSH primarily drives follicular growth in the beginning phases of menstrual cycles. FSH induces multiple follicles to begin development and estrogen secretion. Although multiple follicles develop, usually only one dominates and reaches maturity. Meanwhile, rising estrogen provides negative feedback to decrease FSH production.
LH: The Ovulation Trigger
The LH surge produces the most dramatic hormonal event in the monthly cycle. The surge happens when estrogen is at a critically high level in terms of duration. Due to this, the LH surge causes ovulation about ten to twelve hours after. Furthermore, LH transforms the exhausted follicle into the corpus luteum, which secretes progesterone.
Inhibin hormones provide secondary feedback control throughout the menstrual cycle. Inhibin B dominates in the follicular phase, whereas inhibin A becomes high in luteal phase. Such hormones help in fine-tuning FSH and LH secretion for proper cycling function. Inhibins are therefore important but underappreciated menstrual cycle hormones.
Also Read : Menstrual Cycle: Complete Guide to Phases
Menstrual Hormones and Mood Swings

Neurochemical Mechanism of Estrogen
Hormonal changes during the menstrual cycle are likely to influence mood and emotional state strongly. Estrogen has been found to influence the production of neurotransmitters, especially serotonin and dopamine. Therefore, low estrogen levels can contribute to depression and anxiety symptoms. Also, estrogen withdrawal can lead to irritability and emotional lability.
Progesterone also has multi-faceted effects on mood varying in different individuals to a considerable extent. While progesterone has a sedative effect, its metabolites produce anxiety. Furthermore, abrupt withdrawal of progesterone before menstruation is likely to produce mood symptoms. Furthermore, progesterone affects GABA receptors in the mind, which influence relaxation and sleeping.
PMS: The Hormonal Rollercoaster of Moods
Premenstrual syndrome (PMS) clearly demonstrates the close connection between period hormones and mood. Research indicates that approximately three-quarters all women have one or more PMS symptoms during the luteal phase. Symptoms typically appear after ovulation and disappear with the onset of menstruation. Moreover, severe PMS significantly affects daily functioning and relationships.
Cortisol, the stress hormone, also participates in interaction with menstrual cycle hormones that impact mood. Chronic stress interferes with regular hormone secretion and can enhance PMS symptoms. Elevated cortisol levels are also found to bring on cycle irregularities and moods. Stress management is required to maintain hormonal balance and stable moods.
Also Read : Natural Family Planning: 6 Fertility Secrets
Hormonal Regulation of Menstruation
The HPO Axis: Central Command
The hypothalamic-pituitary-ovarian axis is involved in hormonal control of menstruation by feedback. The intricate process maintains hormone balance through positive and negative feedback. Negative feedback reduces production when hormone levels are excessively high. Positive feedback increases production when levels are excessively low.
Control of the menstrual cycle begins in the hypothalamus through pulsatile release of GnRH. Pulse frequency and amplitude vary across the cycle. In the follicular phase, pulses of GnRH are released every sixty to ninety minutes. Pulse frequency varies during different phases of menstrual cycles.
Pituitary-Ovarian Communication
The pituitary gland, having received the signals from GnRH, then releases adequate amounts of FSH and LH. These hormones circulate in the blood throughout the body to reach the ovaries. The ovarian follicles, in return, release estrogen and eventually progesterone. The release of these hormones completes the cycle of regulation.
Endocrine disruptions may result in a variety of menstrual cycle disorders that should be treated. Polycystic ovary syndrome (PCOS) is a regulatory disorder of hormones. Thyroid disorders also play a significant role in hormonal regulation of the menstrual cycle. Therefore, proper diagnosis and treatment of regulatory disorders are required.
Conclusion
Understanding the role of hormones in the menstrual cycle provides women with more control over their reproductive health. These complex hormonal mechanisms control all aspects of the monthly cycle from timing to symptoms. In addition, understanding normal variations in hormones provides women with the knowledge of when expert medical advice should be sought.
The intricate interaction between progesterone, estrogen, LH, and FSH creates the normal but individualized pattern of the menstrual cycle. In addition, the supporting hormones like inhibins and prostaglandins govern the process. Therefore, hormone balance through healthy living maintains the cycle in top working order.
Disturbances in hormones can have a serious impact on quality of life through many physical and emotional symptoms. Most hormonal symptoms are, however, readily curable with the right medical intervention. The women with distressing symptoms should therefore seek medical practitioners for appropriate evaluation and treatment.